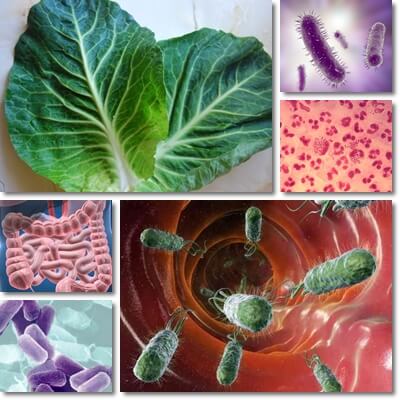
Understanding what is E. coli. E. coli is short for Escherichia coli and is a Gram-negative bacterium, shaped like a rod, non-spore forming, that can grow and multiply both in the presence and absence of oxygen. It populates the gastrointestinal system of humans, mammals and birds and can be expelled in the environment via stools. Most E. coli strains are part of the normal gastrointestinal flora and some of them are good for us, helping produce vitamins, for example. But some strains are disease-causing and produce infections of the gastrointestinal tract with hemolytic uremic syndrome complications, urinary tract infections and skin infections, but also pneumonia and even meningitis in newborns.
Because it’s a Gram-negative bacterium, E. coli has two cell walls which better protect it from immune system cells and make it more resistant to the action of certain antibiotics. The outer cell membrane of E. coli contains a lipopolysaccharide with a lipid A compound which acts as a toxin – when immune system cells try to break down the bacteria cell wall, toxins are released from inside the cell. Side effects include abnormally low blood pressure, abnormally rapid breathing and rapid heart rate, fever or a too low body temperature and either high white blood cell count or a too low white blood cell count. In addition to producing toxicity in response to the action of immune system cells, pathogenic E. coli is more resilient to certain antibiotics because of its double membrane.

Because its double membrane better protects it from certain antibiotics, doctors are very careful what antibiotics they recommend for E. coli infections. For infections such as mild gastroenteritis, some doctors advise against antibiotic therapy if symptoms are manageable, the person was previously healthy with no history of chronic illness or immunodeficiency, is an adult and the infection does not progress to complications. In any case, if you suspect a bacterial gastroenteritis from contaminated food or water or exhibit symptoms of other types of infections, it’s best to see your doctor for an assessment, symptoms management recommendations and treatment. If symptoms get progressively worse, seek medical help immediately. Complications from E. coli infections are more likely in children, the elderly and anyone with chronic diseases or immunodeficiency. The rest of the article is concerned with the symptoms, progression, treatment options and prevention of gastrointestinal E. coli infections.
How does E. coli make you sick?
If a certain number of bacteria are ingested via contaminated water, food or from dirty hands, the bacteria travel to the intestinal tract where they establish themselves and start to grow and multiply. They eventually form colonies and disrupt the normal gastrointestinal flora. Pathogenic E. coli bacteria may use their flagella (lash-like projections they use to move around) and attach themselves to the intestinal wall. As they secure themselves to the intestinal wall, they also wear out microvilli, the innate microscopic projections that stand out on the surface of the intestinal walls and help with nutrient absorption. This also causes inflammation in the cells that line the surface of the intestinal wall and produces damage. Pathogenic E. coli bacteria prevent water absorption and cause diarrhea. Because of the toxins they produce and their infiltration in intestinal cells, E. coli bacteria may also lead to diarrhea with blood.
Another way E. coli makes you sick is when the bacteria multiply and try to overwhelm the natural intestinal flora and take over the gastrointestinal tract. The immune system gets word of the infection spreading and sends immune system cells to eliminate the bacteria. But because they are Gram-negative bacteria and have two cell walls, as the immune system cells try to decompose the bacteria walls, toxins from within the bacteria cell are released, worsening the infection and producing symptoms such as fever, elevated heart rate, abnormally fast breathing or low blood pressure. These toxins can infiltrate in the intestinal lining or worse, escape into the abdomen and cause peritonitis, into other organs resulting in organ failure or into the bloodstream causing extensive infection and even sepsis.
E. coli infection symptoms include
1) Diarrhea – loose, watery stools occurring with great frequency (several times per hour).
2) Abdominal cramps from diarrhea.
3) Blood in diarrhea – a serious symptom indicating severe infection.
4) Nausea and vomiting.
5) Fever, although not always present.
6) Fatigue, malaise, muscle weakness, sleepiness – caused by dehydration from diarrhea and vomiting.
7) Blood in urine, low urine output – signs of severe infection (hemolytic uremic syndrome); require you see a doctor as soon as possible.
E. coli symptoms – how long to show up?
Depending on the strain of E. coli picked up and the age and health of the person prior to the infection, symptoms of an E. coli gastrointestinal infection may show up in as little as 24 hours following exposure or may take as long as 7 days to appear. The average duration from infection to symptoms (incubation time) is 3-5 days.
How long does a gastrointestinal E. coli infection last?
The infection may last anywhere from 3-10 days. Symptoms should improve starting with day 3-5. If you start to feel sick after 5-10 days of infection (when symptoms were beginning to improve) or if your symptoms become progressively worse and don’t improve at all, it is possible there are complications and you should see a doctor as soon as possible.
Possible complications of an E. coli gastrointestinal infection
1) Hemolytic uremic syndrome: It is a medical emergency. Symptoms include:
– Anemia from destruction of red blood cells caused by the toxin produced by certain E. coli strains
– Kidney failure from the red blood cells being eliminated through the kidneys and overwhelming them
– Blood in urine (read more about Urine Colors and What They Mean)
– Abnormally low levels of platelets (blood components that function as coagulation factors) in the blood
– Swelling (edema), high blood pressure, kidney damage, fatigue, confusion and possibly heart attack, blood clots, stroke, seizures, neurological damage, coma.
2) Peritonitis: if there is an ulcer or a perforation somewhere along the intestinal tract, the bacteria may escape into the abdomen and cause peritonitis.
3) Sepsis with symptoms such as abnormally low blood pressure, fast breathing and fast heart rate, edema (swelling), confusion, blood clotting abnormalities and organ failure.
4) Dehydration. The most common complication of a gastrointestinal E. coli infection is dehydration caused by diarrhea and vomiting (read more about Dehydration: Causes and Symptoms). The loss of electrolytes (potassium, magnesium, calcium, sodium), the inability to retain water and other fluids can leave the person dehydrated, feeling fatigued, weak or sleepy. Because of its life-threatening potential, dehydration is the first most important symptom to manage in a gastrointestinal E. coli infection, one that may determine the outcome of the infection, its severity and duration.
How do you get E. coli?
How E. coli spreads is primarily through stool matter from sick people or animals. Examples:
1) Direct, person to person contact: You can pick up the infection from direct contact with a sick person who doesn’t wash their hands after using the toilet.
2) Indirect contact with contaminated objects or surfaces: Any object or surface has the potential to be contaminated with stool matter from a sick person or, in the case of kitchen utensils and surfaces, from contaminated food too (also with stool matter). If you don’t wash your hands before eating or preparing food, you too are at risk of catching the bacteria.
3) Contaminated water. All untreated water and spring water in particular has the potential of being a carrier of pathogenic bacteria like E. coli.
4) Contaminated food. Vegetables and fruits can be contaminated with E. coli as a result of irrigation with untreated sewage water or greywater, use of manure or presence of domestic or wild animals carrying the bacteria in fields. Raw meat, milk and dairy can be contaminated if the animals providing them were sick. All food can be contaminated as a result of a lack of good hygiene during harvesting, processing, transportation, handling or preparation, from people or objects and surfaces.
5) Zoos and petting animals. Contact with stool matter can transmit E. coli further to people.
How is E. coli treated?
Actually, not all gastrointestinal E. coli infections are treated. Although they are bacterial infections, antibiotics are not always recommended, especially for the strains that produce toxins. This is done to limit toxicity of the bacteria in response to the antibiotics, prevent antibiotics resistance and reduce disease duration. Even antidiarrheal agents are contraindicated in the case of certain strains and the diarrhea and vomiting left to continue to help the body get rid of the bacteria faster. Gastrointestinal E. coli infections in previously healthy individuals are self-resolving and only require management of dehydration. This is done by drinking water, teas, electrolyte solutions, even sports drinks or pasteurized fruit juices. If you can eat, do eat light foods, preferable mashed like baby food and pasteurized.
If symptoms get worse, complications occur or the sick person is a child, an older person or someone with a chronic illness or immunodeficiency, seeing a doctor is imperative. The doctor will assess your health and then recommend the best course of treatment for you. Don’t let symptoms worsen for these risk categories and seek medical help from the start.
E. coli – how to prevent infection
Essentially by practicing good hygiene and this includes:
1) Wash your hands well after using the toilet, before eating, preparing food.
2) Separate meat from produce in the refrigerator.
3) Use different cutting boards and kitchen utensils for meat and produce you eat raw. Wash dishes, boards and kitchen utensils well with warm soapy water after each use.
4) Wash fruits and vegetables well before eating; don’t feed raw or unwashed fruits and vegetables and green, leafy vegetables (which are difficult to wash properly) to small children – the risk of infection is high. Choose pasteurized produce and juices for small children.
5) Cook meat and fish well on both sides; don’t feed undercooked or raw meat or fish to small children, pregnant women, the elderly or immunodeficient persons.
6) If there is suspicion a certain food may have caused an E. coli infection, avoid eating that food for a while until the authorities have had time to recall problematic products.
7) Always drink safe water, never from untreated or untested sources like natural springs.
